aetna better health of louisiana prior authorization
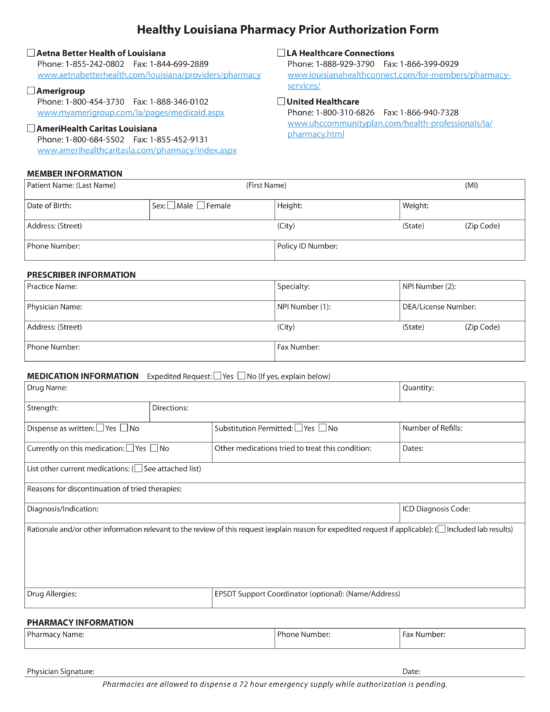
For Pharmacy Benefit Authorization. Please check the members appropriate health plan listed below.
Amerihealth Caritas Louisiana Provider Manual Appendix Manualzz
Medical Management Policy Number.
. Block Vision performs Vision Utilization Management services on behalf of Aetna Better Health Louisiana. They can get the full list on their Provider Portal. AETNA BETTER HEALTH OF LOUISIANA Prior Authorization PA list No authorization is required for emergency services.
Aetna Better Health of Louisiana 2400 Veterans Memorial Blvd Suite 200 Kenner LA 70062 1-855-242-0802. The Peer Supports Services. Vendor will be identified if the criteria was purchased.
Prior Authorization Effective Date. Aetna Better Health of Louisiana. And were here for members statewide in all 64 parishes.
Aetna better health responsibilities the chief medical officer cmo is responsible for directing and overseeing the aetna better health prior authorization of aba. Ama 710005 prior authorization la statement of objective page 1 8110. Medical Management Policy Number.
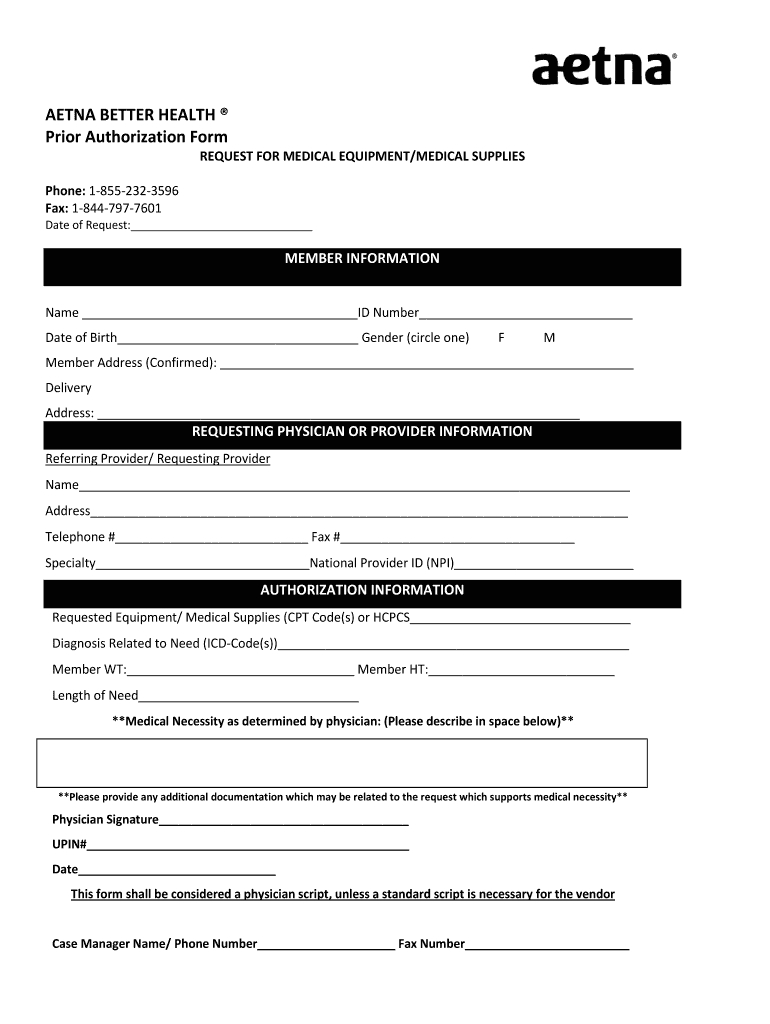
To receive prior authorization from the FI or the MCO the following documentation must be sent for each request. Become a member Your path to better health A wide range of benefits and services can help you get healthier. Peer Support Services Page.
Please contact Block Vision for prior authorization and benefit information of these services by calling 1-866-819-4298. All behavioral health medical director discussions and actions including discussions between medical directors and treating practitionersproviders are to be. Retroactively effective to 11012020- Aetna Better Health of Louisiana will no longer use Eviti for oncology decision support and treatment guidelines.
Please contact DentaQuest for prior authorization and benefit information of these servics by calling 1-855-242-0802. Your provider must check to see if PA is needed before they provide the service. Aetna better health will identify the source of the medical management criteria used for the review of service authorization requests including but not limited to the.
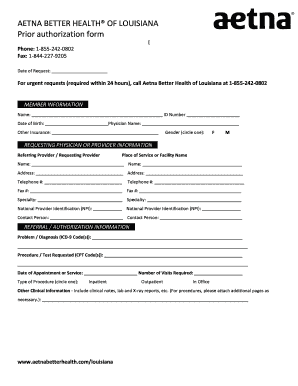
Association or society will be identified if the criteria are developedrecommended or endorsed by a national or state. Aetna Better Health of Louisiana. For urgent requests required within 24 hours call aetna better health.
2 of 9 Department. PHYSICAL HEALTH STANDARD PRIOR AUTHORIZATION REQUEST. Aetna Better Health of Louisiana You deserve to be a leader in your own care.
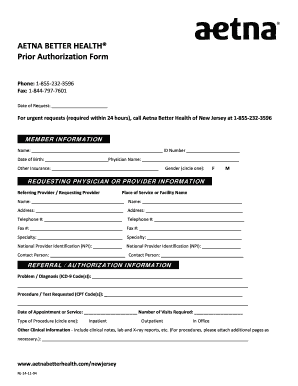
Prior authorization form. You can get the most current list too. Were here 24 hours a day 7 days a week.
Fax the request to 1-844-227-9205 using the Prior Authorization Form. The PDHC prior authorization PA form is standardized regardless of the health plan covering the services. 1 of 11 Department.
Aetna better health prior authorization form. _____ For urgent requests required within 24 hours call Aetna Better Health of Louisiana at 1-855-242-0802. This document represents the majority of services requiring authorizationPlease refer to the code specific listing for details.
There are several options to request an authorization. Healthy louisiana pharmacy clinical criteria pdf link to pdf. Provider An institution or.
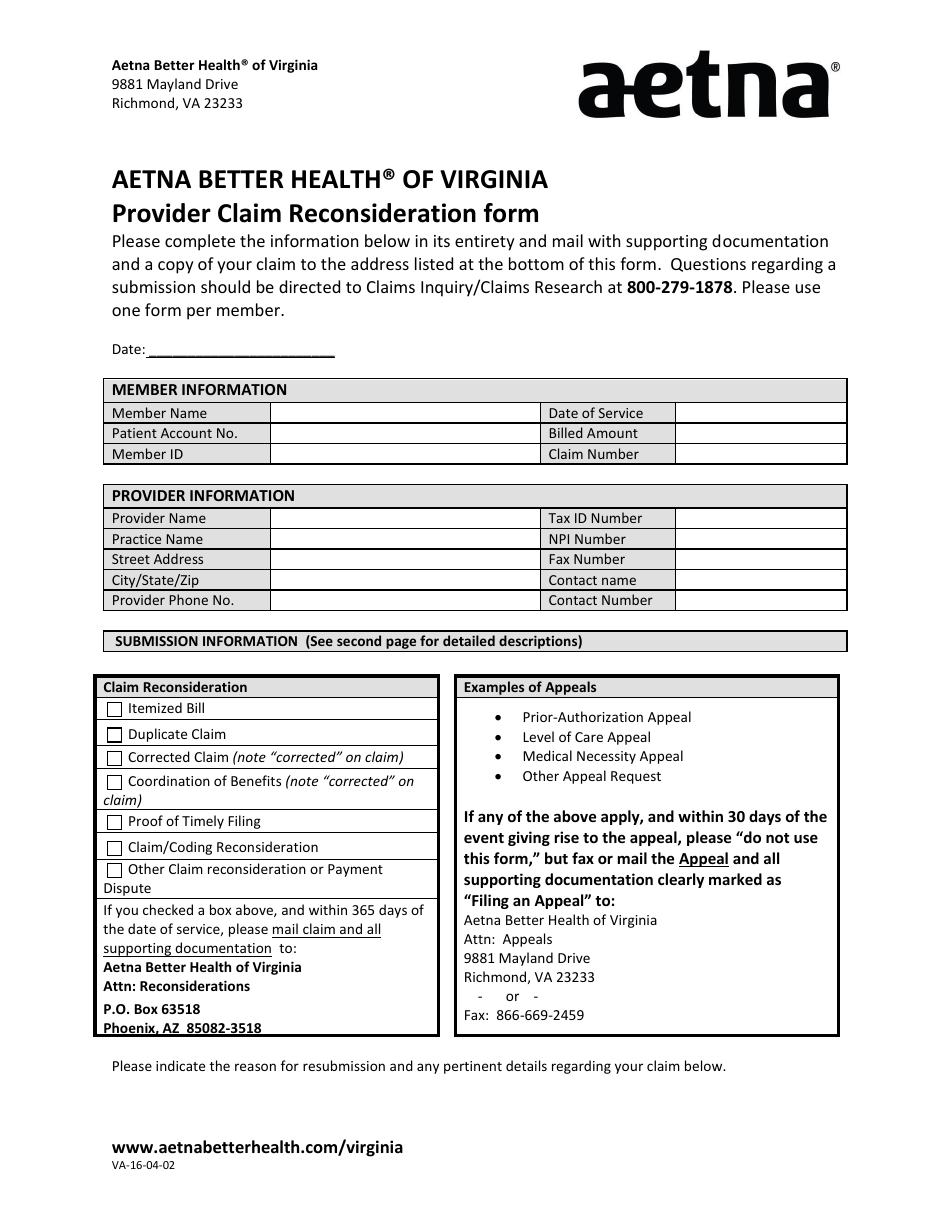
Prior Authorization Prior assessment that proposed services such as hospitalization are appropriate for a particular patient and will be covered by Aetna Better Health. PRIOR AUTHORIZATION REQUEST COVERSHEET. AETNA BETTER HEALTH dba Aetna Better Health of Louisiana.
AETNA BETTER HEALTH dba Aetna Better Health of Louisiana Policy. Dba Aetna Better Health of Louisiana Policy Policy Name. Aetna better health of louisiana.
Or call us at 1-855-242-0802 TTY. The assessment includes a complete history and ongoing assessment of. Medicaid Health Plans MEDICAL MANAGEMENT.
AETNA BETTER HEALTH OF LOUISIANA 2400 VETERANS MEMORIAL BLVD STE 200 KENNER LA 70062 TELEPHONE NUMBER. 1-844-227-9205 Behavioral Health Fax. Easily fill out pdf blank edit and sign them.
Were a state-contracted health plan that offers Healthy Louisiana services. For detailed information refer to the Provider Manual. Prior Authorization Effective Date.
For medical benefit authorizations. A BHLA will process the requests following standard protocol. This guide is intended to be used for quick reference and may not contain all of the necessary information.
Prior authorization is a pre-service or prospective decision. A comprehensive person- centered needs assessment must be completed within thirty 30 days of admission to the program. Providers should visit Prior Authorization Page for more information.
Payment for services depends on whether the patient and the category of service are covered by the members benefit plan. Just check your member handbook on our Member materials and forms page. Use ABHLAs 247 Secure Provider Web Portal.
Applied Behavior Analysis Page. Use a cover sheet with the practices correct phone and fax numbers to safeguard the members protected health information and to facilitate processing. Assertive Community Treatment ACT requires prior authorization and can authorized by Aetna Better Health UM clinicians for up to six 6 months.
Provider Quick Reference Guide.
Aetna Prior Authorization Form For Medication Diigo Groups

Behavioral Health Aetna Better Health Of Louisiana
Preferred One Prior Authorization Form Form Ead Faveni Edu Br
Aetna Referral Form Fill Online Printable Fillable Blank Pdffiller

Prior Authorization Aetna Medicaid Louisiana

Aetna Prior Authorization Form Radiology Fill And Sign Printable Template Online Us Legal Forms

Prior Authorization Aetna Medicaid Louisiana

Ent Referral Letter Fill Online Printable Fillable Blank Pdffiller

Aetna Better Health Of Louisiana Pain Management Program Update Kr2 Medical Billing